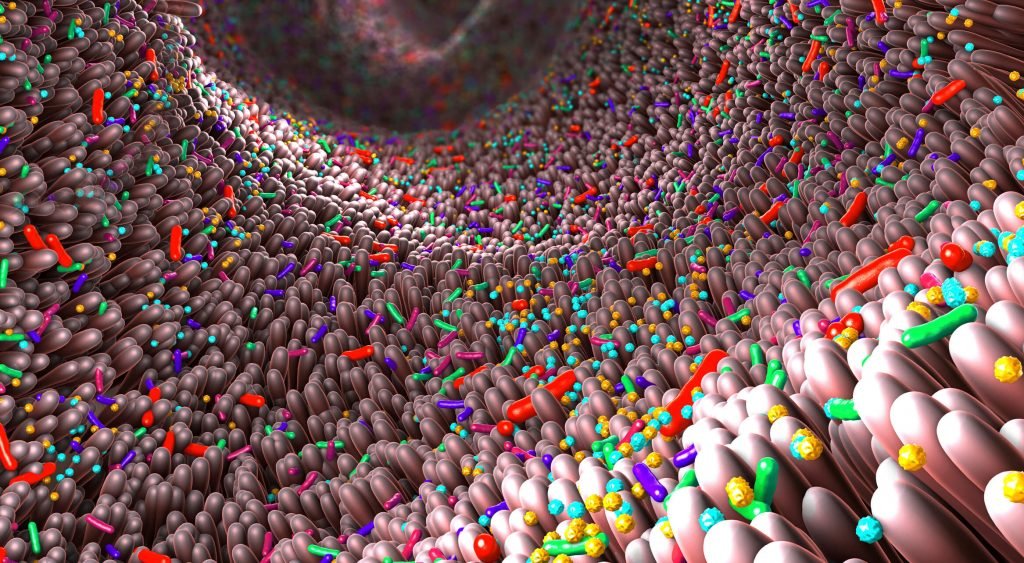
A patient’s gut microbiome may be linked to the risk of developing long-haul COVID-19 after initial infection with SARS-CoV-2, according to a study published online in the journal Gut.1
Although most people with COVID-19 recover within weeks of infection, some experience symptoms 4 or more weeks after COVID-19, according to the Centers for Disease Control and Prevention. These long-haul COVID conditions are also known as post-COVID, long COVID, post-acute COVID-19, long-term effects of COVID, or chronic COVID.2
Huang et al have reported that up to 75% of patients hospitalized with COVID-19 described at least 1 symptom 6 months after discharge.3 These included respiratory, neuropsychiatric (headache, dizziness, loss of taste and smell, anxiety, poor concentration, disrupted sleep, low mood, poor memory, blurred vision), gastrointestinal, hair loss, and musculoskeletal symptoms as well as fatigue.
Continue Reading
Although the exact cause of long-haul COVID-19 is unknown, there is increasing evidence that gut dysbiosis is linked to the severity of COVID-19 infection and persists after disease resolution.4 Microbiome profiling might help identify those patients who are most susceptible to developing long-haul COVID, researchers have theorized.
To further investigate this relationship, Liu and colleagues studied changes in the gut microbiome of 106 patients followed for 6 months after hospital admission for SARS-CoV-2 infection and compared with those of 68 patients without COVID-19. Among the 106 patients with COVID-19, stool samples were collected on admission (68), after 1 month (64), and after 6 months (68); stool samples were also collected from 11 of these patients 9 months later.
The researchers checked for the presence of the 30 most commonly reported long-haul COVID symptoms 3 and 6 months after initial COVID-19 infection. Aerobic capacity and endurance were measured in a 6-minute distance walk test. The average age of the patients with COVID-19 infection was 48 years; just over half were women. The vast majority of patients (81%) had mild to moderately severe infection; 25 were treated with antibiotics.
Study Results
Long-haul COVID was reported in 86 (81%) of the study group at 3 months and in 81 (76.5%) at 6 months. The most common symptoms at 6 months were fatigue (31%), poor memory (28%), hair loss (22%), anxiety (21%), and sleep disturbances (21%). No significant differences were found in potentially influential factors such as age, gender, prevalence of underlying conditions, use of antibiotics or antiviral drugs, or COVID-19 severity between patients with and without long-haul COVID at 6 months postinfection. Among the 68 patients with COVID-19 whose stool samples were analyzed at 6 months, 50 had long-haul COVID.
The microbiome of long-haul COVID-19 patients differed from that of infected patients without long COVID and those without COVID-19 infection. “Gut microbiome of patients with PACS [postacute COVID-19 syndrome] were characterized by higher levels of Ruminococcus gnavus, Bacteroides vulgatus, and lower levels of Faecalibacterium prausnitzii,” said the researchers. “Butyrate-producing bacteria, including Bifidobacterium pseudocatenulatum and F prausnitzii showed the largest inverse correlations with PACS at 6 months,” the researchers reported.
The researchers also examined the makeup of the gut microbiome to see if it was associated with different categories of long-haul COVID-19 symptoms. Eighty-one bacterial species were associated with different categories of long-haul COVID-19 and many species were associated with greater than 2 categories of persistent symptoms, noted the researchers. “Persistent respiratory symptoms were correlated with opportunistic pathogens such as Streptococcus anginosus, Streptococcus vestibularis, Streptococcus gordonii, and Clostridium disporicum. Neuropsychiatric symptoms and fatigue were correlated with nosocomial gut pathogens, including Clostridium innocuum and Actinomyces naeslundii [all P <0.05],” reported the researchers.
Several immune-boosting gut bacteria were found to be depleted in patients with long-haul COVID-19 including B pseudocatenulatum, F prausnitzii, Roseburia inulinivorans, and Roseburia hominis at 6 months.
The gut microbiome of infected patients who didn’t develop long COVID showed only 25 changes in bacteria species at hospital admission, and these alterations returned to normal levels after 6 months. In COVID-19 patients who fully recovered, “baseline gut bacterial composition was enriched in 19 bacterial species and characterized by the genera including Bifidobacterium, Blautia, and Bacteroides.”
The study had some limitations. It was an observational study with only a small number of participants. The study findings will need to be confirmed in larger cohorts across different populations, wrote the researchers.
“This is the first study to demonstrate persistent gut dysbiosis at 6 months after recovery from COVID-19 and a link between altered gut microbiota and common lingering symptoms,” concluded the authors. “Specific gut microbiome profiles were associated with the presence of PACS, suggesting that the human gut microbiome may play an important role in the development of PACS. Considering the millions of people infected during the ongoing pandemic, our findings are a strong impetus for consideration of microbiota modulation to facilitate timely recovery and reduce the burden of postacute COVID-19 syndrome,” they concluded.
References
1. Liu Q, Wing Yan Mak J, Su Q, et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut. 2022;Epub ahead of print: January 26, 2022. doi:10.1136/gutjnl-2021-325989
2. Centers for Disease Control and Prevention. Evaluating and caring for patients with post-COVID conditions: interim guidance. CDC website. Accessed January 31, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-index.html
3. Huang C, Huang L, Wang Y, et al. Six-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220-232. doi: 10.1016/S0140-6736(20)32656-8
4. Chen Y, Gu S, Chen Y, et al. Six-month follow-up of gut microbiota richness in patients with COVID-19. Gut. 2021. [Epub ahead of print: April 8, 2021]. doi:10.1136/gutjnl-2021-324090
This article originally appeared on Clinical Advisor